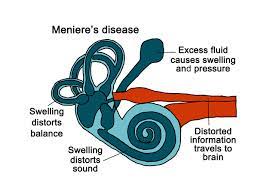
 Kembara Xtra - Medicine - Ménière Disease A condition of the inner ear (labyrinthine) characterized by recurring episodes of hearing loss, tinnitus, vertigo, and feelings of fullness in the ears Ménière Disease is defined by the international diagnostic criteria as a condition with at least two spontaneous episodes of vertigo lasting longer than 20 minutes but less than 12 hours, an audiogram demonstrating evidence of low- to medium-frequency sensorineural hearing loss in one ear at any given time, and fluctuating aural symptoms like hearing loss, tinnitus, or aural fullness. Clinically, it includes the following three symptoms: - Vertigo that lasts 20 minutes to 12 hours - Sensorineural hearing loss (predominantly low frequency) as determined by audiometry - Variable auditory complaints, such as tinnitus or aural fullness Frequently unilateral at first; over time, approximately half turn bilateral. While vertigo severity and frequency may lessen over time, hearing loss is frequently progressive and/or variable. Menière syndrome, which might be related to another disorder that causes endolymphatic hydrops, is typically idiopathic (Ménière disease). Both unilateral and bilateral diseases can be divided into 5 different clinical subgroups. Classic unilateral MD and metachronic bilateral MD (symptoms first present in one ear, then the other) are considered to fall under Type 1. - Type 2: describes delayed unilateral MD (hearing loss begins months or years before vertigo begins) or synchronic bilateral MD (both ears experience symptoms at the same time). Type 3: Family-based MD Even while unilateral patients might coexist in the same family (the majority of families have bilateral hearing loss), Type 4: Sporadic migraine-related MD Type 5: Sporadic autoimmune disease-related MD Nervous system(s) damaged; endolymphatic hydrops; Ménière syndrome Epidemiology: Predominant age of onset: 40 to 60 years; females outnumber men (2:1); and Northern Europeans of white race are superior to blacks. Estimated annual incidence ranges from 1 to 150/100,000. Variations in prevalence from 7.5 to >200/100,000 Pathophysiology and Etiology Unknown; ideas include higher endolymph fluid pressure brought on by increased fluid production or decreased resorption. This could be brought on by inflammation brought on by circulating immune complexes, aberrant vestibular aqueduct development, or endolymphatic sac pathology. Changes in the endolymphatic ionic gradient and membrane rupture may result from increased endolymph pressure. Vascular compromise, cochlear damage, viral infection, or reactivation are a few additional major hypotheses. Injury or other conditions, such as diminished middle ear pressure, allergies, endocrine disorders, lipid disorders, vascular, viral, syphilis, or autoimmune diseases, may contribute to Ménière syndrome. Ménière syndrome could be caused by any condition that could result in endolymphatic hydrops. Genetics Though the influences of genetic and environmental factors are not fully understood, some families exhibit greater incidence. Stress, allergies, increased salt intake, caffeine, alcohol, or nicotine, chronic exposure to loud noise, family history, and genetic susceptibility are all potential risk factors. Autosomal dominant inheritance is present in 10% of cases. Certain viral exposures, especially those that result in herpes simplex virus [HSV], certain vascular abnormalities (including migraines), and Prevention Reduce your exposure to established risk factors such stress, ototoxic medicines like aspirin, quinine, and aminoglycosides, as well as your intake of salt, alcohol, and caffeine. Associated Conditions Migraines, Hyperprolactinemia, Hypothyroidism, Anxiety (due to the incapacitating symptoms), Diagnosis A clinical diagnosis is made. History Symptomatic episodes are usually unprovoked, but they could be accompanied by tinnitus and a developing aura of ear fullness. These can come in groups and have protracted periods of symptom-free remission. According to the American Academy of Otolaryngology-Head & Neck Surgery's official criteria for diagnosis: - At least two bouts of vertigo lasting more than 20 minutes, which are typically characterized by rotating or rocking feelings. - Aural fullness or tinnitus - Low frequency (sensorineural) hearing loss is verified by audiometric testing. - Exclusion of additional causes, such as acoustic neuromas - Pallor, sweating, nausea, vomiting, falling, and prostration may happen during severe bouts. clinical assessment Physical examination eliminates other diseases; Ménière disease-specific findings are not made. During assaults, horizontal nystagmus could be visible. Otoscopy is frequently uncomplicated. As vertigo is often of shorter duration and induced by head movements in BPPV, the diagnosis of benign paroxysmal positional vertigo (BPPV) rather than Ménière illness is suggested by the occurrence of attacks in the workplace with the Dix-Hallpike maneuver. Differential diagnosis: Endolymphatic sac tumor, transient ischemic attack (TIA), migraine, acoustic neuroma or another CNS tumor, syphilis, viral labyrinthitis, other labyrinthine disorders (such as Cogan syndrome, benign positional vertigo, and temporal bone trauma), vertebrobasilar disease, vestibular neuronitis, diabetes or thyroid dysfunction, otitis media Laboratory Results Testing is conducted to eliminate the possibility of other illnesses, but it does not always confirm or rule out Ménière disease. Consider serologic tests that are specific for Treponema pallidum in at-risk populations as initial tests (lab, imaging). Studies on lipids, fasting blood sugar, and thyroid To rule out an auditory neuroma or other CNS pathology, such as a tumor, aneurysm, or multiple sclerosis (MS), consider getting an MRI. Other/Diagnostic Procedures The auditory system uses pure tones and speech to demonstrate low-frequency sensorineural (nerve) loss and reduced speech discrimination; this method typically reveals low-frequency sensorineural hearing loss. - Weber and Rinne tests, ABR, or MRI to rule out an acoustic neuroma - Electrocochleography may be helpful to determine the cause. Vestibular-caloric testing: While not diagnostic in and of itself, decreased activity on either side is compatible with the diagnosis of Ménière disease. - Testing for head impulses Interpretation of Tests Histologic examination of the temporal bone (during autopsy); dilated inner ear fluid system, thickening of the basement membrane, loss of hair cells, and perivascular microvascular damage Cytochemical examination can show altered cochlin and mitochondrial protein expression, as well as altered AQP4 and AQP6 expression in the supporting cell. DTNA and FAM136A genes have been linked to familial Ménière illness. Management There are few evidence-based recommendations, and medications are typically used to treat the symptoms of nausea and vertigo. During attacks, bed rest with the eyes closed helps prevent falls. Attacks rarely persist longer than four hours. Basic Prevention Since the 1929 articles by Dederding and Mygind and the 1934 Furstenberg trial, the salt restriction diet has been the principal first-line treatment for MD. Since the 1950s, this approach has been defended and criticized in a number of publications, and the data supporting it is still up for debate. First Line of Medicine Acute attack: Initial objectives are symptom alleviation and stabilization; for severe episodes - Benzodiazepines, such as diazepam, reduce anxiety and vertigo - Meclizine/dimenhydrinate antihistamines: lessen nausea and vertigo - Anticholinergics (transdermal scopolamine): lessen motion sickness-related nausea and emesis - Antidopaminergic medications (promethazine, metoclopramide): reduce nausea and anxiety - Rehydration treatment and replacing electrolytes - Tapering of steroids for severe hearing loss A low-salt diet is one necessary modification in lifestyle for maintenance (the aim of which is to prevent/reduce attacks). - By lowering endolymphatic pressure and volume, diuretics may help prevent attacks, however there is insufficient data to support routine use: Hydrochlorothiazide; triamterene/hydrochlorothiazide (Dyazide, Maxzide) Betahistine, a weak histamine H1 agonist and a greater histamine H3 antagonist, is frequently used in Europe in place of the acetazolamide (Diamox) drug (unavailable in the US) (7). The evidence on the usefulness of other vasodilators, such as isosorbide dinitrate, niacin, and histamine, is inconclusive. Warnings and contraindications: - Atropine: prostatic enlargement, supraventricular tachycardia, and other arrhythmias, as well as heart illness - Scopolamine: prostatic hypertrophy in the elderly and children - Renal disease, electrolyte imbalances, and diuretics Sedatives should only be used with extreme caution, especially in older patients. Patients are advised not to operate machinery or automobiles. In particular, care should be taken when using atropine and scopolamine. Diuretics: Keep an eye on electrolytes. Significant potential interactions with transdermal scopolamine include tricyclic antidepressants, anticholinergics, and antihistamines. Next Line Systemic and intratympanic (PO or IV) steroids have been used to treat hearing loss for a longer period of time: In one pilot research, prednisone 30 mg/day added to diuretic therapy decreased the severity and occurrence of tinnitus and vertigo. There is little evidence to support the usual use of Famvir; it may help hearing more than balance. Dexamethasone is practical to employ since patients tolerate it better than methylprednisone. Consider referring patients to ear, nose, and throat specialists or neurologists. Patients should undergo official audiometry to confirm hearing loss. Further Treatments Vertigo can be reduced by utilizing a Meniett device to provide intermittent pressures via a myringotomy (8)[B]: Safe; long-term tympanostomy tube is necessary. The international consensus on the treatment of MD suggests that vestibular rehabilitation should be made available as a treatment option for patients between vertigo crises. Vestibular rehabilitation may be advantageous for patients with persistent vestibular symptoms. It is safe and effective for unilateral vestibular dysfunction. Surgical Procedures Hearing-preserving Interventions: - Endolymphatic sac surgery was beneficial in reducing vertigo in 75% of Ménière disease patients who had not responded to medication treatment. - Intracranial surgery to cut the vestibular nerve Tympanostomy tube: this procedure may lessen symptoms by lowering middle ear pressure. It is more intrusive, but it reduces vertigo and preserves hearing. Treatments for patients whose hearing is not functional: - Labyrinthectomy, which is quite effective at reducing vertigo but results in hearing loss - Endoscopic vestibular nerve section - Vestibular neurectomy - Implantation of a cochlea Alternative Therapies Numerous integrative therapies, such as acupuncture, acupressure, tai chi, niacin, bioflavonoids, lipo-flavonoids, ginger, Ginkgo biloba, and other herbal supplements have all been explored despite the lack of solid evidence to support their efficacy. Patient Follow-Up Monitoring It is crucial to keep an eye on changes in hearing as well as to keep an eye out for more serious underlying reasons (such an acoustic neuroma), as there is a chance that progressive hearing loss may occur despite a decrease in vertiginous events. Diet Unless certain foods trigger attacks, diet rarely comes into play. Patients should be informed about the likelihood of remissions and attacks occurring in succession. The patient may be totally functional between episodes, but their activity is frequently restricted by dread or residual sensations. This may make you completely disabled. 90% of cases can be successfully managed with medicine; 5-10% of patients need surgery for incapacitating vertigo. Severity and frequency of attacks reduce, although hearing loss is frequently progressive. Some instances continue >20 years. Complications hearing loss, attack-related injuries, and employment incapacitation
0 Comments
Leave a Reply. |
Kembara XtraFacts about medicine and its subtopic such as anatomy, physiology, biochemistry, pharmacology, medicine, pediatrics, psychiatry, obstetrics and gynecology and surgery. Categories
All
|


 RSS Feed
RSS Feed
