|
Clinical Procedures - Barium Enema • The following refers to the standard 'double contrast' barium enema. Indications • Investigation of colonic pathology. Indications include pain, melaena, anaemia, palpable mass, change in bowel habit, failed colonoscopy, investigation of remaining colon in the case of a known colonic tumour • • Always consider alternatives (e.g. colonoscopy, CT colonography). Contraindications • Absolute: lack of informed consent, possible perforation, pseudomembranous colitis, toxic megacolon, biopsy via rigid sigmoidoscope within 5 days, biopsy via flexible endoscope within 1 day •Relative: barium meal within 7-14 days, patient frailty or immobility: • • The procedure requires a large amount of patient cooperation. The patient must be able to lie flat and to turn over easily • The patient must be able to retain rectal barium and air. Procedure The colon is coated with barium, then inflated with air and images are taken from several different angles. Performed by a radiographer or radiologist. • The patient lies in the left lateral position on the fluoroscopy table • The operator may perform a digital rectal examination before beginning • A rectal tube is placed, attached to a bag of barium sulphate. The barium is run into the colon under x-ray guidance until it reaches the right colon • The barium is drained • IV buscopan or, if contraindicated, glucagon is given • The colon is inflated with air (or with CO, in some centres) • The patient is instructed to roll and is tilted as images are acquired • Once the images are obtained, the colon is deflated and the patient can go to the bathroom to empty their bowel and shower if necessary • The examination may last 15-30 minutes • The patient should be kept in the department until any medication side effects (e.g. blurred vision) have worn off. Risks • Perforation (increased risk in elderly, ulcerating lesions, systemic steroids, hypothyroidism, large bowel obstruction): • Intraperitoneal barium causes hypovolaemic shock and a 50% mortality. Of those that survive, 30% have adhesions • Cardiac arrhythmia (secondary to the large bowel distension) • Medication effects Patient Preparation • Iron tablets: stop 5 days before • Constipating agents: stop 2 days before • Fasting: low residue diet 2 days before, fluids only on the day before • Bowel preparation: laxative (usually Picolax® taken at 08:00 and 18:00 on the day before. Other Information • Buscopan is given to inhibit intestinal motility. Side effects include blurred vision, dry mouth, and tachycardia: Contraindicated in angina, untreated closed-angle glaucoma, prostatic hypertrophy, myasthenia gravis, paralytic ileus, and pyloric stenosis • Glucagon is given if buscopan cannot. Risk of hypersensitivity and is contraindicated in phaeochromocytoma, insulinoma, and glucagonoma • After the procedure, the patient may eat and drink as usual but is advised to keep their bowel moving to avoid barium impaction • A barium study will prevent a CT examination of the same area for a period of time as intestinal barium creates dense streak artefact. Water-Soluble Contrast Examinations • In the case of recent surgery, suspected perforation, or investigation of a leak, water-based iodinated contrast is used instead of barium. Examples include Gastrografin®, Urografin®, Niopam®, Omnipaque® • A single-contrast examination is performed (i.e. the colon is not inflated with air) and many of the standard' views are not included • No bowel preparation or fasting is needed.
0 Comments
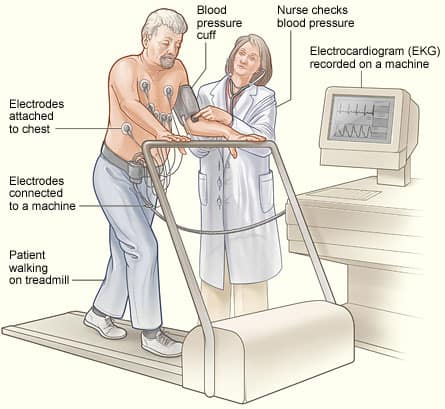
Clinical Procedures - Barium Follow-Through Indications • Investigation of small bowel pathology, particularly suspected Crohn's disease and strictures. Indications include pain, diarrhea, malabsorption, partial obstruction, anemia • D Always consider alternatives (e.g. MRI, small bowel enema). Contraindications • Absolute: lack of informed consent, complete small bowel obstruction, suspected perforation (a water-soluble contrast may be used instead). Procedure The patient drinks barium and the small bowel is intermittently imaged until the barium has reached the caecum. Usually performed by a radiologist. • The patient is given a mixture of barium to drink • The exact mixture given to the patient varies between centres and between radiologists. Some add Gastrografin® to the barium, which has been shown to reduce transit time. Many add 20mg of metoclopramide to the mixture which enhances gastric emptying • Once the barium has been consumed, the patient is asked into the fluoroscopy room and images are taken of the small bowel with the patient lying supine • Real-time fluoroscopy is employed to assess small bowel motility • Images are taken every 20-30 minutes until the barium has reached the colon • The radiologist may use a 'spoon' or similar radiolucent device to press on the patient's abdomen to separate loops of bowel • Additional images of the terminal ileum are usually obtained, often with the patient supine and many radiologists also acquire an 'overcouch' plain abdominal radiograph with compression applied to the lower abdomen • The time taken depends on the small bowel transit time and, although usually an hour, patients are advised to allow up to 3 hours • After the procedure, the patient may eat and drink as usual but is advised to keep their bowel moving to avoid barium impaction. Risks • Leakage of barium through an unsuspected perforation: • Intraperitoneal barium causes hypovolaemic shock and a 50% mortality. Of those that survive, 30% have adhesions • Barium impaction (causing large bowel obstruction) or barium appendicitis • Medication effects Patient Preparation • Fasting: nil by mouth for 12 hours before the examination • Bowel preparation: laxative (usually Picolax®) taken 12 hours before. Other information • Metoclopramide aids gastric emptying. Extra-pyramidal side effects may occur, especially in young women and there is a risk of acute dystonic reactions such as oculogyric crisis. Contraindicated in patients with Parkinsonism/Parkinson's disease • D A barium study will prevent a CT examination of the same area for a period of time as intestinal barium creates dense streak artefact. Clinical Procedures - Barium Swallow/Barium Meal Barium swallows examine the oropharynx, oesophagus, and GO]; barium meals examine the stomach and first part of the duodenum. They are often performed together as described below. Indications • Investigation of esophageal and gastric pathology. Indications include dysphagia, odynophagia, dyspepsia, weight loss, anaemia, epigastric mass, partial obstruction • I Always consider alternatives (e.g. OGD, MRI). Contraindications • Absolute: lack of informed consent, complete bowel obstruction, suspected perforation (a water-soluble contrast may be used instead) • Relative: a large degree of patient cooperation is required so those unable to understand or follow instructions are unsuitable. Also, the patient must be able to stand for the duration of the examination and to lie supine if necessary. Procedure The patient drinks barium whilst the esophagus and stomach are imaged fluoroscopically. Usually performed by a radiologist. • The patient stands in the fluoroscopy machine • A gas-producing agent is ingested (e.g. Carbex®) and the patient is asked not to belch • Images are taken as the patient swallows mouthfuls of barium. The patient must be able to hold the liquid in their mouth and swallow on command • Once views of the esophagus have been obtained, the machine is tilted so the patient is supine. The patient is instructed to roll and tilt as images of the stomach are obtained from several angles: • This requires a certain degree of patient fitness • The time taken depends to a degree on how easily the patient follows the commands, although usually lasts 15-20 minutes • After the procedure, the patient may eat and drink as usual but is advised to open their bowels regularly to avoid barium impaction. Risks • Leakage of barium through an unsuspected perforation: • Intraperitoneal and intramediastinal barium has a significant mortality rate • Barium impaction (causing large bowel obstruction) or barium appendicitis. Patient Preparation • Fasting: nil by mouth for 6 hours before the examination • Bowel preparation: none required • Smoking: patients are asked not to smoke for 6 hours before the procedure as this increases gastric motility. Other Information • A barium study will prevent a CT examination of the same area for a period of time as intestinal barium creates dense streak artefact. Water-Soluble Contrast Examinations • In the case of recent surgery, suspected perforation, or investigation of a leak, water-based iodinated contrast is used instead of barium. Examples include Gastrografin®, Urografin®, Niopam®, Omnipaque® • A single-contrast examination is performed (i.e. the gas-producing agent is not given and many of the 'standard' views are not included • In contrast to the barium examinations, these studies can be carried out on patients who are frail and/or have recently had surgery • Intraperitoneal or intramediastinal water-soluble contrast does not carry the risks of barium but aspiration of the contrast can result in pulmonary edema and lung fibrosis. Hypersensitivity is also a risk. Clinical Procedures - Colonoscopy Indications • Diagnostic: gastrointestinal bleeding, iron-deficiency anemia, chronic diarrhoea, lower abdominal symptoms (chronic constipation, lower abdominal pain, bloating), evaluation of known inflammatory bowel disease (IBD), surveillance for cancer (in IBD patients/after colonic polypectomy/ after curative intent resection of colorectal cancer), screening for colorectal cancer • Therapeutic: polypectomy (including endoscopic mucosal resection techniques: EMR), angiodysplasia treated with argon plasma coagulation (APC), decompression of volvulus or pseudo-obstruction, dilatation, or stenting of strictures or malignant colonic obstruction. Contraindications • Absolute: lack of informed consent, toxic megacolon, fulminant colitis, colonic perforation •Relative: acute diverticulitis, symptomatic large abdominal aortic aneurysm, immediately post-op, recent MI or PE, severe coagulopathies: • Colonoscopy can be performed safely in pregnancy but should be deferred in most instances unless requiring immediate resolution. Procedure Colonoscopy is an endoscopic examination of the mucosal surface from the anal canal to the terminal ileum. • Patient lies on the couch in the left lateral position with knees bent • Endoscopist first performs a digital rectal examination • Sedation (e.g. midazolam) may be given with monitoring of oxygen saturation. IV analgesia (e.g. pethidine) is also given: • Increasing use of either no sedation (with improved techniques such as 'Scopeguide®') or inhaled nitric oxide • Lubricated colonoscope (about 12mm wide and 185cm long) is passed rectally. Air is insufflated. Water-jet may also be used via the scope • Aim is to pass to the terminal ileum • Duration varies but averages at about 20 minutes. Risks • Perforation (0.2-0.4% diagnostic; higher with therapeutic procedures) • Bleeding (1 in 1000) • Abdominal distension, medication effects (allergic reactions, nausea vomiting hypotension, respiratory depression) • Rarities: infection, postpolypectomy coagulation syndrome: (pain, peritoneal irritation, leucocytosis and fever), splenic rupture, small bowel obstruction. Patient Preparation • Iron and constipating agents: discontinue iron tablets 7 days and constipating agents 4 days prior to the procedure • Anticoagulant and antiplatelet therapy: in the case of a planned polypectomy or other therapeutic procedure, refer to BS guidelines on the management of anticoagulant and antiplatelet therapy (www.bsg. org.uk) • Antibiotic prophylaxis: none for colonoscopy. See other topics for comparison • Bowel preparation: the colon must be empty. Protocols vary but usually include prescribing 1 sachet of sodium picosulfate (Picolax®) for the morning and afternoon of the day before procedure. Other Information • The introduction of the bowel cancer screening programme has meant that endoscopists need to pass a 'driving test' to demonstrate high-level competency to perform safe screening colonoscopy •EMR is used for larger or difficult flat polyps. The lesion is lifted by submucosal injection of gelofusin, adrenaline, and dye followed by snare resection. Polyps can then be retrieved by 'Roth' baskets for histological assessment. Clinical Procedures - Esophagogastroduodenoscopy Indications • Diagnostic: haematemesis, dyspepsia (>55 years old), oesophageal and gastric biopsies (?malignancy), duodenal biopsies (?coeliac), surveillance (e.g. Barrett's oesophagus), persistent nausea and vomiting, iron-deficiency anemia, dysphagia • Therapeutic: treatment of bleeding lesions, variceal banding and sclerotherapy, stricture dilatation, polypectomy, endoscopic mucosal resection, palliative intent (e.g. stent insertion, laser therapy), argon plasma coagulation for suspected vascular lesions. Contraindications • Absolute: lack of informed consent, possible perforation, haemodynamic instability, hypoxaemia with respiratory distress, uncooperative patient •Relative: pharyngeal diverticulum, recent MI or PE. Procedure • Endoscopic examination of the mucosa of the esophagus, stomach, and proximal duodenum. Allows direct visualization, mucosal biopsies, and other therapeutic procedures • Dentures (if present) are removed • Patient is given anaesthetic throat spray (lidocaine) ‡ IV sedation (e.g. midazolam) • Patient lies on the couch in the left lateral position • Hollow mouthpiece is inserted to protect the patient's teeth and facilitate instrument passage • Endoscope (9.5-12.5mm diameter, max. 120cm long) is slowly advanced and swallowed by the patient • Scope advanced and manipulated by the endoscopist to allow visualization of the target structures • Procedure time varies but average 3-15 minutes. Risks • Minor throat and abdominal discomfort • Cardiorespiratory: arrhythmias, MI, respiratory arrest, shock, death Infection (uncommon, e.g. aspiration pneumonia) Perforation (around 0.03% with a mortality of 0.001% during diagnostic procedures, higher with therapeutic procedures): • Overall 2-3% perforation with esophageal dilatation; mortality 1% • Bleeding (caution with low platelet counts and high INR) • Medication effects including anaphylactic reactions and oversedation • Dental trauma. Patient Preparation • Fasting: 4 hours prior to the procedure unless in an emergency situation • Antibiotic prophylaxis: none for OGD. See other topics for comparison. Other Information • Dosages of benzodiazepines and opiates should be kept to a minimum to achieve sedation, with lower doses being prescribed in elderly patients • The pharynx is sprayed with local anaesthetic spray. There is some evidence that the combination use of local anesthetic spray and IV sedation increases the risk of aspiration pneumonia • Patients who have had IV sedation should not drive, operate heavy machinery, or drink alcohol for 24 hours afterwards. Clinical Procedures - Capsule Endoscopy Indications • Obscure gastrointestinal bleeding (in patients with negative gastroscopy and ileocolonoscopy), known or suspected small bowel Crohn's disease, assessment of coeliac disease, screening and surveillance for polyps in familial polyposis syndromes. Contraindications • Lack of informed consent, intestinal strictures, adhesions, obstruction • Diverticula or fistulae that may block the passage of capsule endoscope • Cardiac pacemakers or other implanted electronic devices • Difficulty in swallowing tablets or known swallowing disorders • Pregnancy (lack of available safety data) • D Patients with obstructive symptoms or known or suspected inflammatory bowel disease should have either a small bowel follow-through or a patency capsule (dissolves after 36 hours), with an abdominal radiograph taken 24 hours after ingestion to identify whether capsule is retained within small bowel: • If retained, capsule endoscopy is not appropriate • D Capsule retention can occur even in the absence of strictures on barium or MR-enteroclysis study. Procedure • The capsule consists of a disposable, wireless, miniature video camera which can be swallowed and passes through the intestine by peristalsis • Images taken by the capsule are transmitted, via sensors secured to the abdominal wall, to a battery-powered data recorder worn on a belt • The capsule leaves the stomach within 30 minutes and the patient is allowed to drink after 2 hours and eat after 4 hours • The external equipment is removed after 8 hours (approximate battery life) by which time the capsule has reached the caecum in 85% of cases • The capsule is expelled naturally after 24 48 hours in the patient's stool • Data from the recorder is downloaded onto a computer workstation which allows approximately 50,000 images to be viewed as a video. Risks • Capsule retention (may cause partial or complete intestinal obstruction; highest risk in patients with extensive small bowel Crohn's disease, chronic usage of non-steroidal anti inflammatory drugs, abdominal radiation injury, previous major abdominal surgery or small bowel resection) • Capsule endoscopy may also fail in patients with dysphagia, gastroparesis, and anatomical abnormalities of the gastrointestinal tract. The external equipment which the patient will wear, consisting of a data-recorder and electrodes. Patient Preparation • Iron supplements: stop taking 1 week prior to procedure • Constipating agents: stop 4 days before the procedure • Fasting: patients are fasted for 8-12 hours prior to the procedure and may receive bowel prep (taken day before procedure). Other Information • Incomplete examination in 10-25% of cases: • Presence of dark intestinal contents in distal small bowel may impair visualization of mucosa • Delayed gastric emptying and small bowel transit can lead to exhaustion of battery life before capsule reaches ileocaecal valve • Capsules are being developed to screen for esophageal varices and may be more 'guided' in future as the technology develops • Positive findings on capsule endoscopy may be reachable using either single- or double-balloon enteroscopy or spiral enteroscopy. Clinical Procedures - Exercise Tolerance Testing (ETT) Indications • Assessment of chest pain in those with known coronary artery disease (there is no longer a role for ETT in patients presenting with chest pain who do not have a history of coronary artery disease) • Assessment of haemodynamic response in those with known valvular disease who are asymptomatic • Diagnosis of exertionally induced arrhythmias or syncope. Contraindications • Any undiagnosed or previously unknown murmur (patient should undergo echocardiogram first) • Severe aortic stenosis (risk of syncope) • Hypertrophic cardiomyopathy with significant outflow obstruction (risk of syncope) • Severe hyper- or hypotension • Unstable angina (should undergo coronary angiography) • Known severe left main stem disease • Untreated congestive cardiac failure • Complete heart block • Aortic aneurysm • Acute myocarditis or pericarditis • Any recent pyrexial or 'flu-like' illness. Procedure • ECG electrodes are put on the patient's chest and a sphygmomanometer cuff on an arm • The patient is asked to walk on a treadmill connected to the computer whilst their ECG, blood pressure, and heart rate are monitored. The speed and incline of the treadmill increase according to set protocols: • Bruce protocol: for assessment of physically fit and stable patients with suspected coronary artery disease, 7 stages starting at a 10% gradient at 1.7mph and increasing to 22% gradient and 6mph • Modified Bruce protocol: used in elderly patients or those who have been stabilized after a suspected episode of unstable angina. Starts at 1.7mph and 0% gradient and increases the gradient slowly to 10% • Termination of the test depends on the results seen (see box). Risks • Risks are those associated with exercise and include: • Arrhythmia, cardiac ischaemia, myocardial infarction, syncope. Patient Preparation • No specific preparation is required. Patients are asked not to eat or drink for 3 hours prior to the test • Comfortable clothing and shoes should be worn. Indications for termination of procedure • Patient requests to stop • Symptoms: fatigue, angina, dizziness, significant breathlessness • Signs: drop in oxygen saturations <94%, target heart rate achieved, hypotension during exercise (e.g. BP <100mmg), significant hypertension (e.g. BP >200mmHg) • ECG: any atrial or ventricular arrhythmia, frequent ventricular ectopics, new AV or bundle branch block, ST segment shift >1mm. Causes of false positive results or low specificity • Often due to difficulty interpreting results as result of resting ST segment abnormalities: •Wolf-Parkinson-White syndrome, left bundle branch block, atrial fibrillation, left ventricular hypertrophy, digoxin therapy, hyperventilation, biochemical electrolyte abnormalities (e.g. hypo- or hyperkalaemia), cardiomyopathies, left ventricular outflow obstruction Beta-blocker therapy prevents the appropriate heart rate/blood pressure response during testing. Clinical Procedures - Echocardiography Indications • Myocardial infarction: assess wall motion and left ventricular function • Valvular heart disease: assess competency and examine prostheses • Embolic stroke: to exclude a cardiac embolic source • Infective endocarditis: look for valvular vegetations • Cardiomyopathy: assess ventricular dilatation/hypertrophy and function • Congenital heart disease • Pericardial disease • Pericardial effusion: distribution of fluid and suitability for drainage • Aortic disease: severity and site of aneurysm, dissection, or coarctation. Contraindications • The only contraindication is lack of patient consent or if the patient is unable to cooperate. Technology • Echocardiography is an ultrasound examination and uses the same technology (and machines) as general ultrasound. See separate topic • Ultrasound becomes increasingly less diagnostic at greater depths and cannot see through lung. Images in large individuals are often suboptimal and the heart may not be seen at all in patients with hyperinflated lungs. Procedure • Time taken will vary depending on examinations performed and complexity of the findings. Most examinations last between 20-25 minutes • With the patient lying on their left side, the operator uses a hand-held probe coated with gel to examine the heart usually via the anterior chest and epigastrium. Risks •There is no published evidence that ultrasound has ever directly caused any harm to a patient • Heating: some equipment can produce temperature rises of 4°C in bone. Most equipment in clinical use is unlikely to increase tissue temperature more than the 1.5°C which is considered 'safe • Non-thermal hazard: ultrasound has been demonstrated to produce tiny gas pockets and bubbles in animal models but there is no evidence that diagnostic ultrasound can cause harm to tissues other than neonatal lung. Patient Preparation • No preparation is required. Other Information: Type of Echocardiography Along with 2-dimensional transthoracic echocardiography, the following methods exist: • 3D: uses computer software to produce a 3-dimensional image. Useful in left-ventricular functional assessment especially post-infarction • 4D: 3D imaging with real-time movement captured • TOE: transoesophageal echo is an invasive procedure. It requires written consent and is performed under sedation with local anaesthetic spray to the upper pharynx. The probe is covered, lubricated, and passed into the esophagus behind the heart. It is used to visualize the posterior cardiac structures. The investigation of choice for infective endocarditis • Stress echo: used to assess myocardial ischaemia at 'rest and during 'stress'. Stress is induced by exercise or (more commonly) by an IV infusion of dobutamine in a controlled environment • Bubble studies: used to assess for intracardiac shunts such as atrial or ventricular septal defects or patent foramen ovale. Air bubbles are agitated in a syringe and injected into a peripheral vein. The Valsalva manoeuvre is performed and, if a shunt exists, bubbles will be seen moving from the right side of the heart to the left. Clinical Procedures - Coronary Angiography/Angioplasty Indications • Diagnostic: unstable or refractory angina, acute coronary syndrome, positive or inconclusive stress testing • Emergency therapeutic: where possible, patients presenting with acute ST-elevation myocardial infarction should have primary coronary intervention rather than thrombolysis • Elective therapeutic: suitable 'target lesion' identified on diagnostic coronary angiogram. Contraindications • Absolute: refusal of patient consent • Relative: acute renal failure, pulmonary edema, known radiographic contrast allergy, uncontrolled hypertension, active gastrointestinal haemorrhage, acute stroke, and untreated coagulopathy. Procedure • Percutaneous access via a guide needle into a peripheral artery (most commonly the radial artery) • Guide catheter is introduced, the tip is placed at the coronary ostium, radio-opaque contrast is injected, and real-time x-ray is used to visualize the blood flow through the coronary • The coronary guidewire is inserted through the catheter into the coronary artery using x-ray guidance • The guidewire tip is passed across the site of stenosis • The balloon catheter is passed over the guidewire until the deflated balloon lies across the target lesion • The balloon is then inflated and compresses the plaque and stretches the artery wall. A stent (wire mesh tube) can be inserted using a similar technique and be left in place maintaining the arterial lumen • The guidewire, catheter, and sheath are carefully removed • The patient should remain supine for 4 hours following the procedure unless an arterial closure device has been used. Risks • Minor: contrast allergy, vasovagal reaction, hemorrhage and hematoma at puncture site, thrombosis formation, false aneurysm, AV fistulation, pulmonary edema, and renal failure due to contrast nephropathy • Major: limb ischaemia, coronary artery dissection, aortic dissection, ventricular perforation, air or atheroma embolism, ventricular arrhythmias failure of procedure, and need to proceed to coronary artery bypass graft • Death (<1 in 1000). Patient Preparation • Pre-procedure check list: written consent, group and save, ECG, check full blood count/clotting/U&Es. Other Information for Junior Doctors • Coronary angioplasty is associated with increased thrombus formation (balloon inflation disrupts the intima, revealing prothrombotic cores of plaques), therefore antiplatelet therapy is necessary • Patients will need to have long-term antiplatelet therapy; usually lifelong aspirin 75mg once daily, but they will also need clopidogrel 75mg once daily (see local guidelines: usually 3 months for bare metal stents and 12 months for drug-eluting stents or angioplasty after acute coronary syndrome) • Patients with renal failure should be carefully considered. lodinated contrast can be nephrotoxic and renal decompensation may occur following coronary angiography/plasty. The risk can be minimized by hydration before and after the procedure. Renal function should be carefully monitored. Check local guidelines. Clinical Procedures – Endoscopic Retrograde Cholangiopancreatography ( ERCP) Indications • Diagnostic: largely superseded by safer modalities such as endoscopic ultrasound and MRI/MRCP. Diagnostic indications include sphincter of Oddi dysfunction and primary sclerosing cholangitis • Therapeutic: endoscopic sphincterotomy (biliary and pancreatic), removal of stones, dilation of strictures (e.g. primary sclerosing cholangitis), stent placement. Contraindications • Lack of informed consent, uncooperative patient, recent attack of pancreatitis, recent Ml, history of contrast anaphylaxis, severe cardiopulmonary disease, futility (anticipated short-term survival with no features of sepsis). Procedure An ERCP involves the passage of an endoscope into the duodenum. The endoscopist injects contrast medium through the ampulla of Vater via a catheter. Real-time fluoroscopy is used to visualize the pancreas and biliary tree. Selected images are taken. • Dentures (if present) are removed • Patient is given anaesthetic throat spray (lidocaine) and sometimes IV sedation/analgesia (e.g. midazolam, pethidine) • Patient lies on the couch in a modified left lateral ('swimmer's") position with the left arm adducted and the right abducted. The endoscope is inserted as for OGD • Under x-ray guidance, a polyethylene catheter is inserted into the biliary tree and contrast instilled to outline the pancreatic duct as well as the common bile duct and its tributaries • Procedure time varies from 30-90 minutes. Risks • Pancreatitis (2-9% of procedures of which 10% of cases are mild-moderate). Serum amylase is temporarily raised in 70% • Infection (ascending cholangitis, acute cholecystitis, infected pancreatic pseudocyst, liver abscess, endocarditis • Bleeding, perforation of the oesophagus, duodenum, bile ducts • Failure of gallstone retrieval • Prolonged pancreatic stenting associated with stent occlusion, pancreatic duct obstruction, pseudocyst formation • Basket impaction around a large gallstone (may require surgery). Patient Preparation • Blood tests: liver enzymes, platelets and clotting are checked prior to the procedure. • Nil by mouth: 4 hours except in the case of an emergency. • Antibiotic prophylaxis: recommended for: • Patients in whom biliary decompression is unlikely to be achieved at a single procedure (e.g. dilatation of dominant stricture in multifocal sclerosing cholangitis or hilar cholangiocarcinoma) • Consider also in patients with severe neutropenia (<0.5 × 109/L) and/ or profound immunocompromise. Other Information • © I sedation and analgesia is usually administered and the back of the throat is sprayed with local anaesthetic • Hilar biliary obstruction demonstrated on MR or CT imaging may be more successfully stented using percutaneous transhepatic cholangiography (PTC) than ERCP • Equipment allowing direct cholangioscopy (with the potential for sampling lesions) is becoming more widely available. |
Kembara XtraFacts about medicine and its subtopic such as anatomy, physiology, biochemistry, pharmacology, medicine, pediatrics, psychiatry, obstetrics and gynecology and surgery. Categories
All
|










 RSS Feed
RSS Feed
